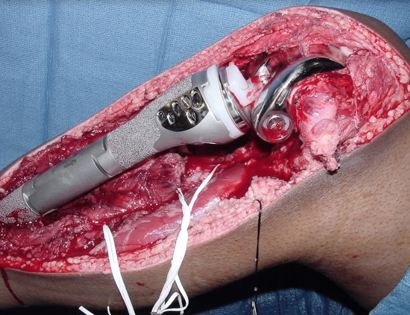
What is a Limb-Sparing Surgery of the Tibia/Knee?
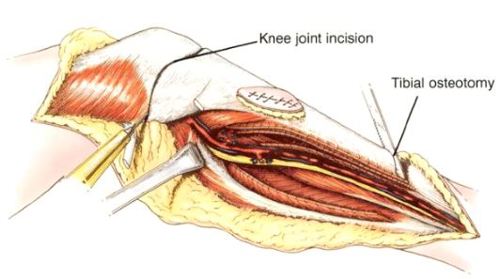
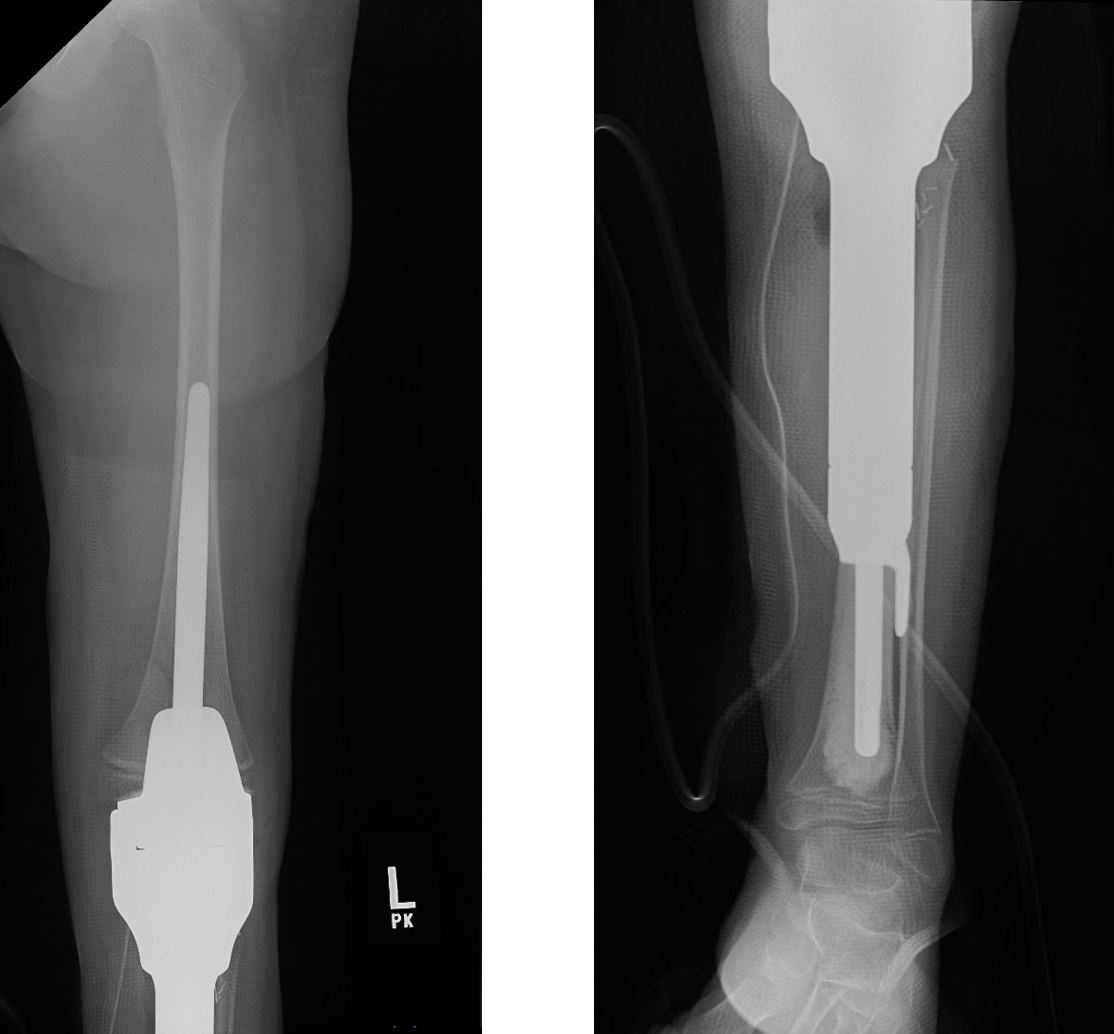
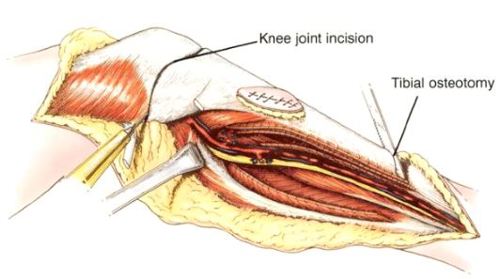
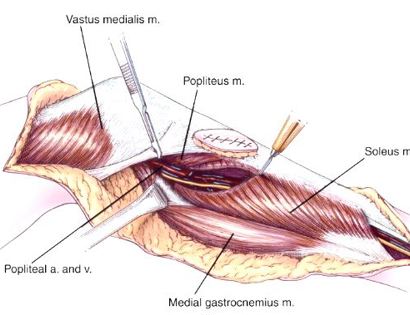
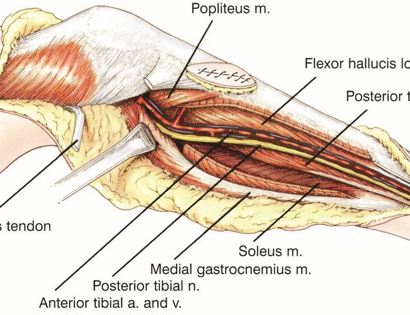
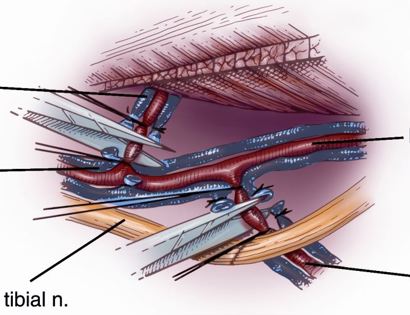
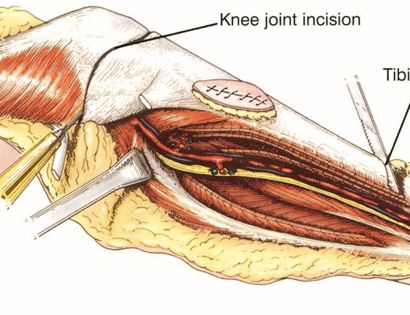
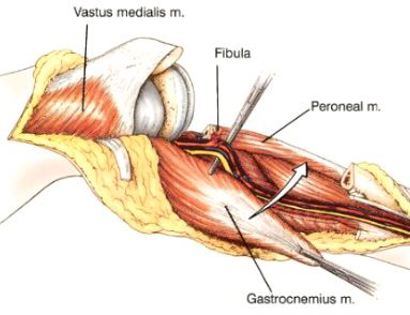
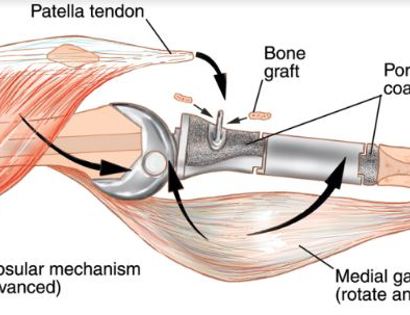
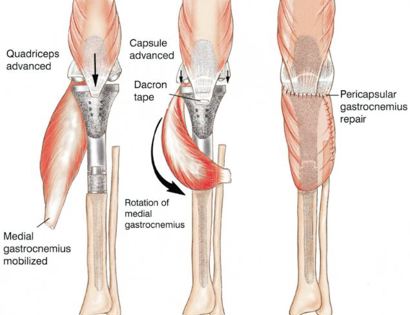
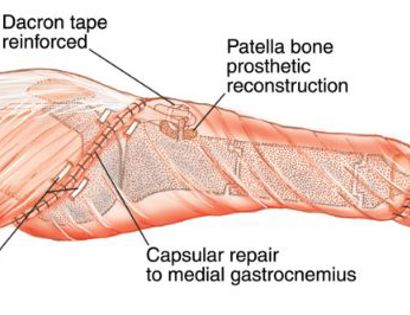
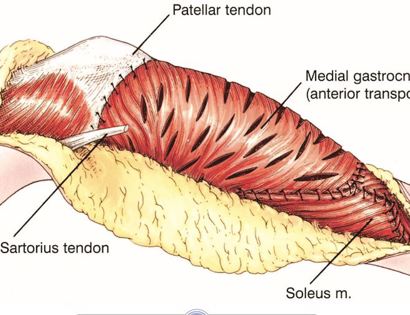
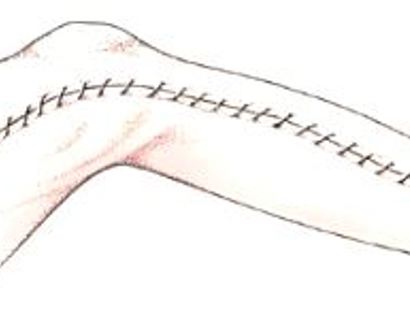
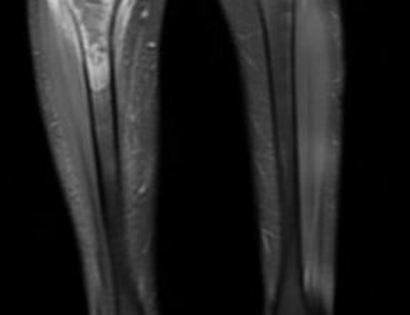
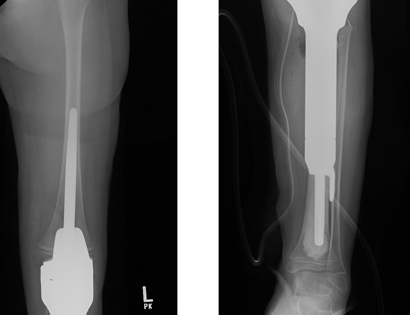
The knee joint consists of your distal femur (lower part of thigh bone), tibia (shin bone), fibula, and patella. The proximal tibia (upper part of shin bone) is a relatively common site for primary bone sarcomas, metastatic disease, and aggressive benign tumors. The common muscles of this area include the gastrocnemius, soleus, and popliteus (calf muscles). Some of the tumors arising in this region include osteosarcomas, ewing’s sarcoma, and giant cell tumor. Limb-sparing surgery can be performed for approximately 95% of tumors arising from the proximal (upper) tibia. In some instances the extremity cannot be saved and a above the knee amputation is performed.
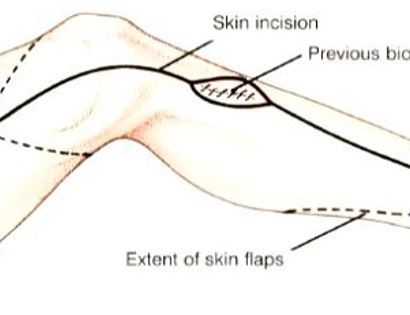
Contraindications for saving the limb may include neurovascular invasion, infection, pathological fracture, invasion of the pelvis, extensive disease, contamination from a poorly performed biopsy, recurrent disease.