Excision of Benign Bone Tumors
It is a procedure that involves removing a tumor (malignant or benign) of the bone while preserving the surrounding healthy bone and soft tissues and reconstructing the defect (space where tumor was removed).
It is a procedure that involves removing a tumor (malignant or benign) of the bone while preserving the surrounding healthy bone and soft tissues and reconstructing the defect (space where tumor was removed).
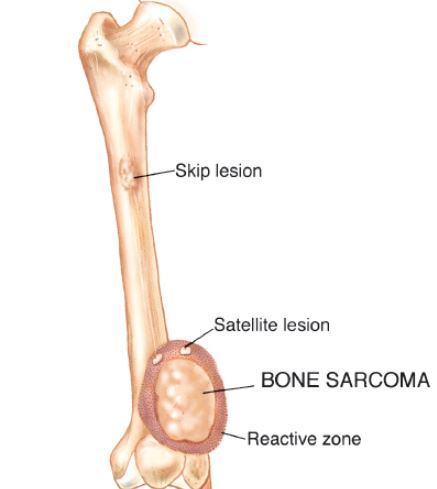
There are a variety of non-cancerous bone tumors, and although benign, some cause pain, grow quickly, and act aggressively. Benign bone tumors are identified on radiographs and definitively diagnosed with biopsies. The bone tumors are further classified into stages, with stage 1 being a latent bone tumor, stage 2 being an active bone tumor that continues to grow and expand, and stage 3 being an aggressive and invasive bone tumor. Commonly, stage 1 benign bone tumors are treated through observation or excision of the lesion, dependent of its nature. Stage 2 benign bone tumors are treated with intralesional excision and reconstructed with local grafting and/or cementation. Lastly, stage 3 benign bone tumors are treated with intralesional excisions or marginal/en bloc excisions and reconstructed with grafting, cementation, endoprosthesis, and/or allograft prosthetic composite. More aggressive tumors, including those that are labeled as high grade, require more aggressive treatment, as these tumors often invade and destroy the bone and surrounding soft tissues. Higher grade bone tumors also have higher recurrence rates, and therefore need a more aggressive and effective treatment. Marginal/en bloc excisions are used to treat bone tumors and diminish recurrence rates by removing adequate tissue (margins) without destabilizing local structures. In this procedure, the surrounding tissue, nerves, and vessels are protected, and tumor is completely removed with the utilization of special tools and instruments. Margins are also taken to prevent recurrences in the future. Afterward, the surgical site is irrigated and then the bone is repaired with bone cement, grafts, or replaced with a prosthesis.
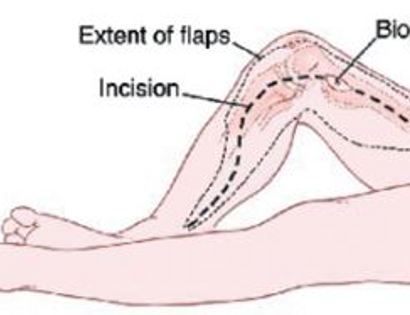
The incision is made, containing the marked biopsy site, along with margins so no tumor remains after it is removed.
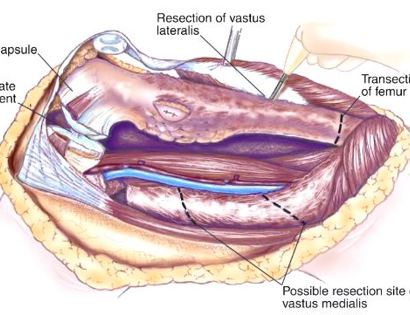
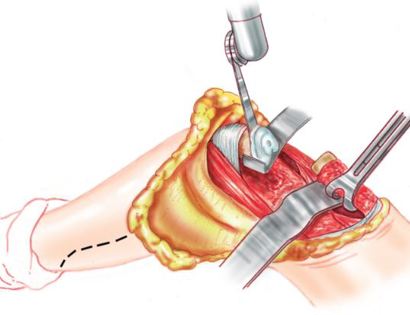
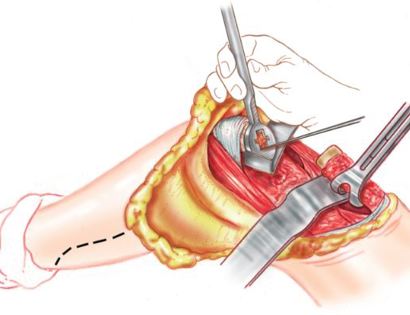
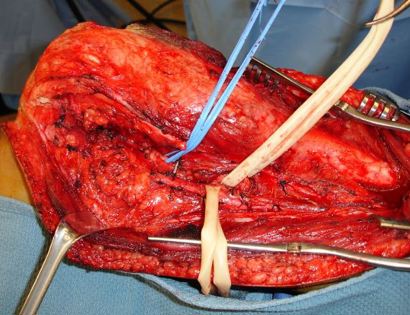
Developing surgical planes (margins that are tumor free) and separating muscles that can be preserved and leaving those in continuity with the tumor that should be removed. This is based on preoperative MRI and intraoperative findings as well as the type of tumor.
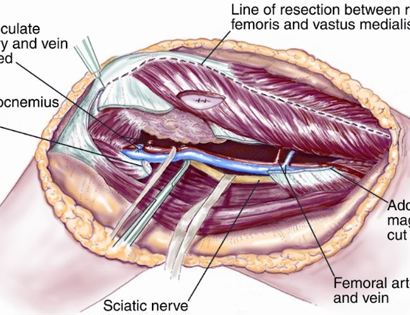
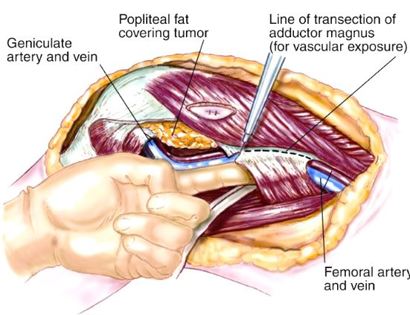
Separating all major arteries, veins, and nerves from the tumor. In rare cases a nerve (s) may need to be removed if it is involved by the bone sarcoma. For this procedure it is vital that the femoral vessels (femur artery and veins), popliteal vessels (arteries and veins around your knee joint), and sciatic nerve are properly identified. Once the blood vessels and nerves are properly identified they can be retracted (moved away) and protected throughout the procedure.
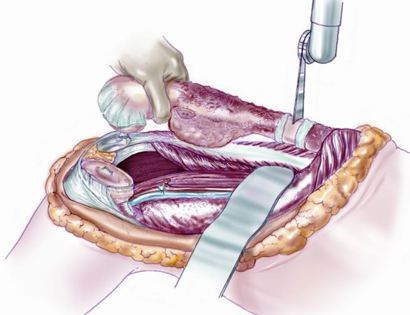
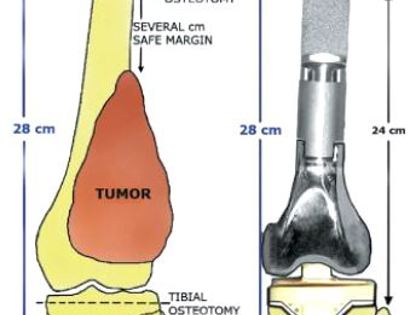
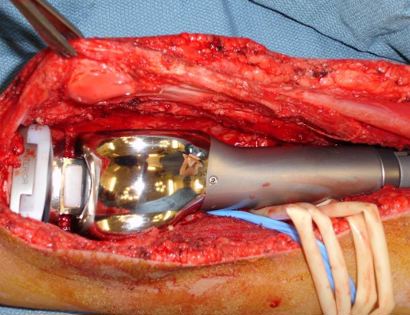
Removal of tumor and reconstruction with a tumor prosthesis. Reconstruction of the lower leg/knee utilizing a specialized tumor prosthesis is the most common limb-sparing technique for bone sarcomas, soft-tissue sarcomas, or large benign aggressive tumors that have destroyed the bone arising in this area. This prosthesis is sized and built during the surgical procedure then implanted and secured in place using cement. The length of bone removed is based on preoperative X-rays and MRI.
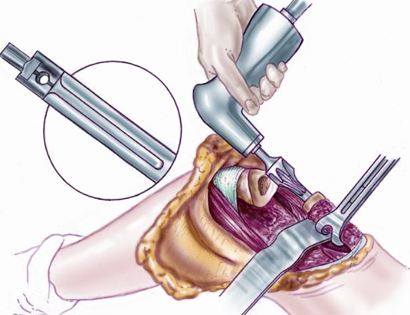
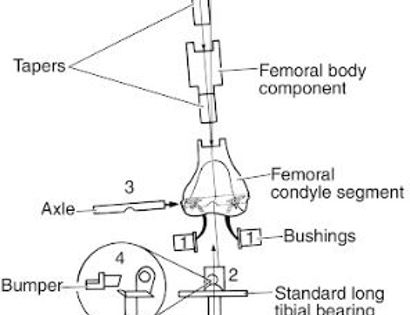

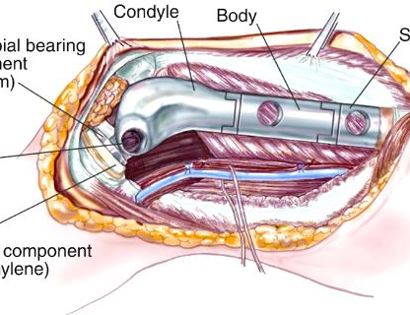
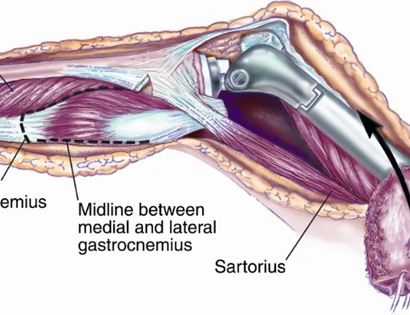
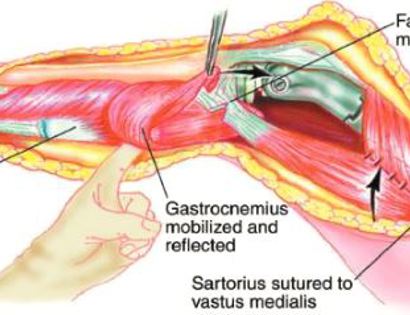
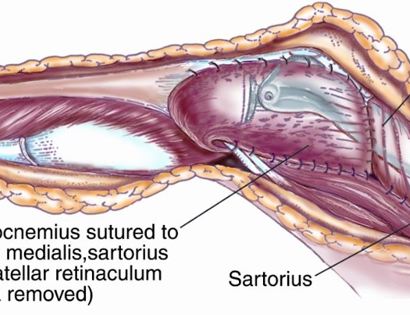
Soft tissue coverage of the prosthesis. Multiple muscle rotation flaps are used to restore function and stability of the knee as best as possible. The goal is to provide a stable knee so the extremity can function well. Soft-tissue reconstruction that involves rotating and reattaching the surrounding muscles, including the gastrocnemius (calf muscle) and vastus medialis (quadriceps muscle). Restoring the function of the surrounding muscles and knee joint is most important for achieving optimal functional outcomes and for protecting the prosthesis from infection.
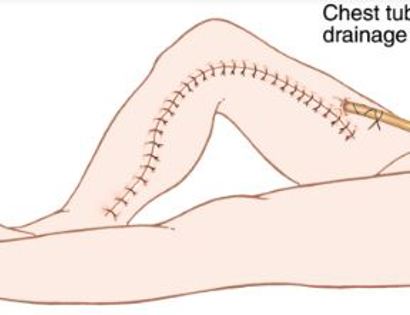
We then close your incision with sutures and cover the surgical site with bandages. Multiple large drains may also be used to drain the surgical site and prevent a seroma (buildup of fluid).








After your surgery you may spend a few nights in the hospital depending on the type of surgery. Once discharged from the hospital, you will be recuperating at home. Various pain protocols and nerve blocks are used to minimize pain. Mostly all patients are very comfortable after the surgery. For the first few days you will ice the area and keep it elevated to reduce swelling. You will return to the office 2 weeks after surgery. Once cleared, you may subsequently start physical therapy depending on the extent of your procedure. We usually prescribe specific physical therapy protocols 3 times a week for 12 weeks after surgery to gradually strengthen muscles. Strengthening with significant resistance after sufficient range of motion is achieved as determined by Dr. Wittig. There may be an ultimate weight limit imposed upon you depending on various factors.
You will be monitored periodically with X-Ray and MRI imaging over the course of 5 years to ensure there are no signs of recurrence. You will have follow up appointments every 4 months for the first 2 years, then every 6 months for the next 2 years, and then once a year. Since the integrity of the limb has been restored to full or almost full, recovery is anticipated provided the patient adheres to strict physical therapy.

Dr. James Wittig narrates a video illustrating the surgical technique for the resection of a bone sarcoma. | WATCH VIDEO