What is Limb Sparing Surgery of the Shoulder Blade/Scapula?
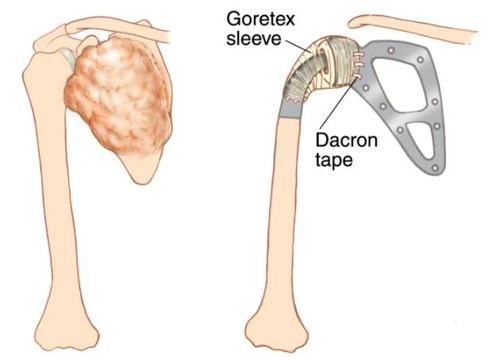
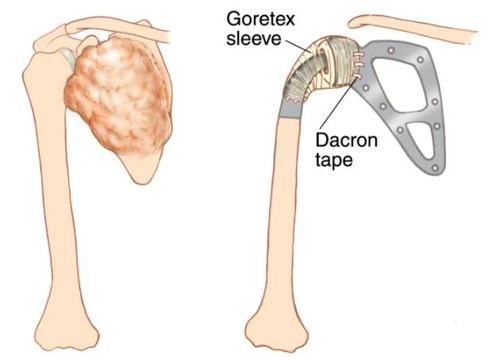
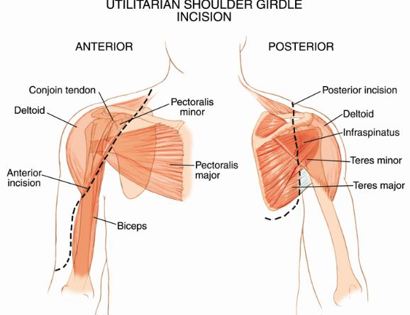
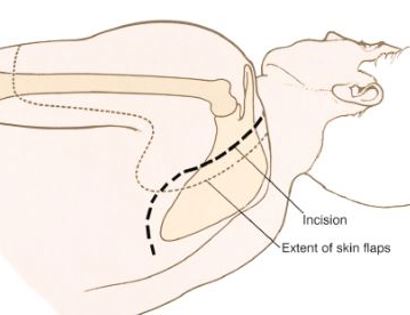
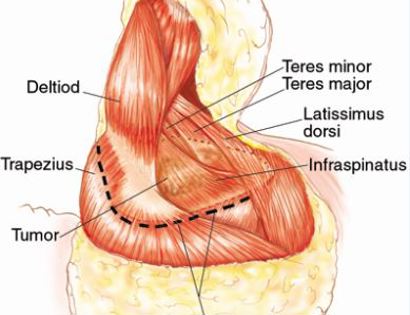
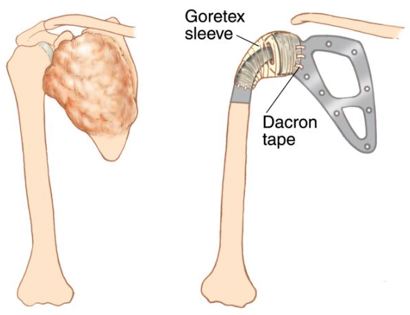
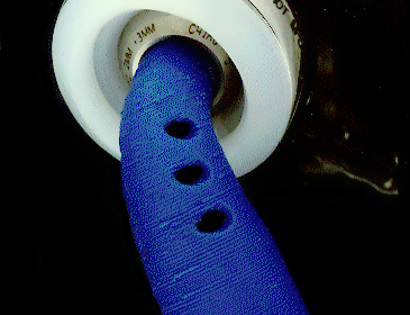
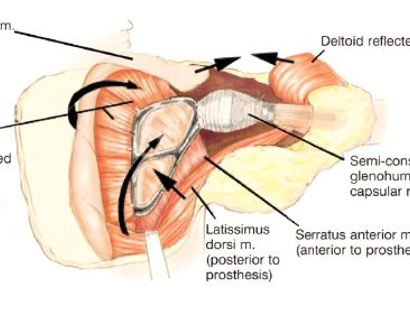
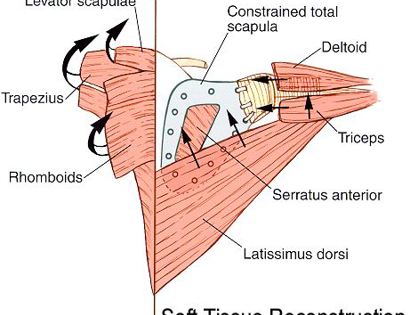
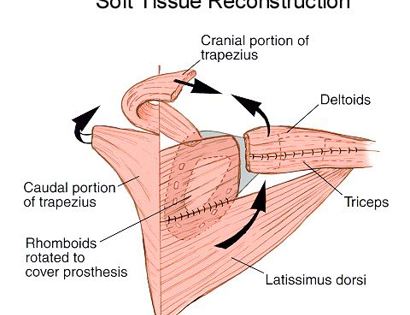
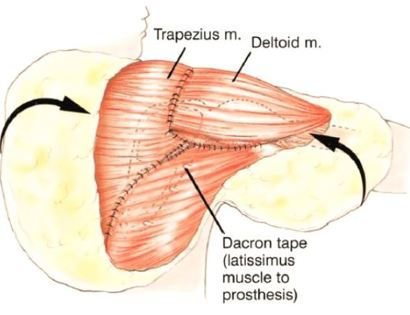
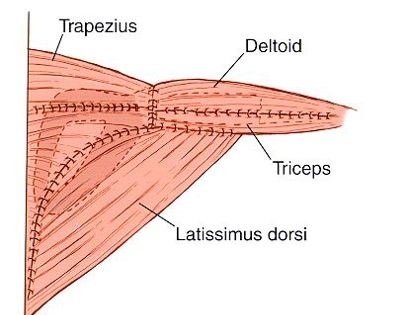
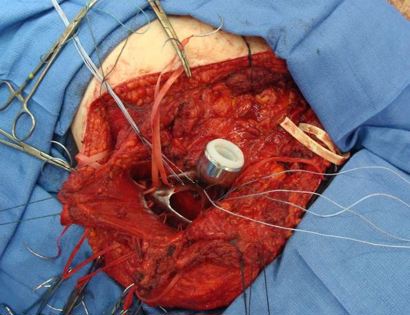
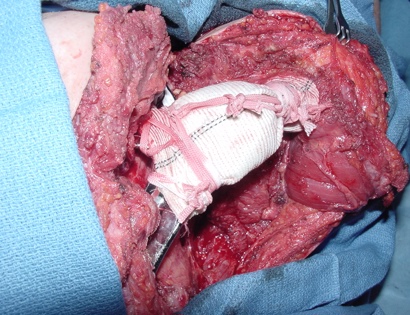
The shoulder girdle, as seen in the figure below, consists of the proximal humerus, scapula, and clavicle. The shoulder joint is formed by the glenoid (cup), which is part of the scapula, and the proximal humerus ball, which is the upper portion of your arm. There are many muscles that attach to your scapula, including the rotator cuff muscles. The scapula, also known as your shoulder blade, is a common site for primary sarcomas to arise. Some of these include chondrosarcoma, osteosarcoma and Ewing’s sarcoma. Soft tissue sarcomas can also develop around the scapula and shoulder, and invade the adjacent bones. Limb-sparing surgery can be performed for approximately 95% of tumors arising from or around the shoulder girdle. In order to reconstruct the shoulder girdle with a total scapula prosthesis one must be able to preserve the deltoid muscle and axillary nerve, trapezius muscle, rhomboids and latissimus. In some instances, the extremity cannot be saved, and a forequarter amputation is performed.
Contraindications for saving the limb may include neurovascular invasion, infection, pathological fracture, invasion of the chest wall, extensive disease, contamination from a poorly performed biopsy, recurrent disease.