Curettage and Midas Rex Burr
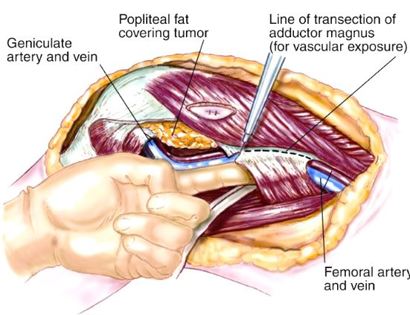
It is a procedure that involves removing a tumor (malignant or benign) of the bone while preserving the surrounding healthy bone and soft tissues and reconstructing the defect (space where tumor was removed).
It is a procedure that involves removing a tumor (malignant or benign) of the bone while preserving the surrounding healthy bone and soft tissues and reconstructing the defect (space where tumor was removed).
Since sarcomas spread microscopically a distance from the main tumor, it is usually important to remove a cuff of surrounding normal tissue around the tumor. The more aggressive the tumor (usually more rapidly growing or called high grade) the wider the margin. Technically, radical means removing the entire bone and muscle that contains the tumor. The extent of the bone sarcoma is determined on the preoperative MRI. Sarcomas should never be removed piece by piece as it will spread the tumor. Also they should not be removed with an intralesional procedure that means entering the tumor and scraping it out of the bone. There are a few exceptions to this rule for some low grade and slow growing sarcomas that are less aggressive and have a much lower risk of coming back than the high grade or rapidly dividing bone sarcomas. Most high grade bone sarcomas are treated with chemotherapy before surgery (preoperative or neoadjuvant chemotherapy) and more chemotherapy after surgery (adjuvant chemotherapy). Radiation is rarely used in the treatment of bone sarcomas. Chemotherapy before surgery is aimed at killing the main tumor as well as any microscopic cells that have traveled in the body. It may also make saving the limb easier with the ability to save more normal tissues around the sarcoma. Sometimes there is major shrinkage of the sarcoma depending on the type of sarcoma. Sometimes a bone sarcoma may be determined to be unresectable meaning it needs an amputation. Preoperative chemotherapy may kill the sarcoma and make it resectable; capable of saving the limb instead of amputating it.
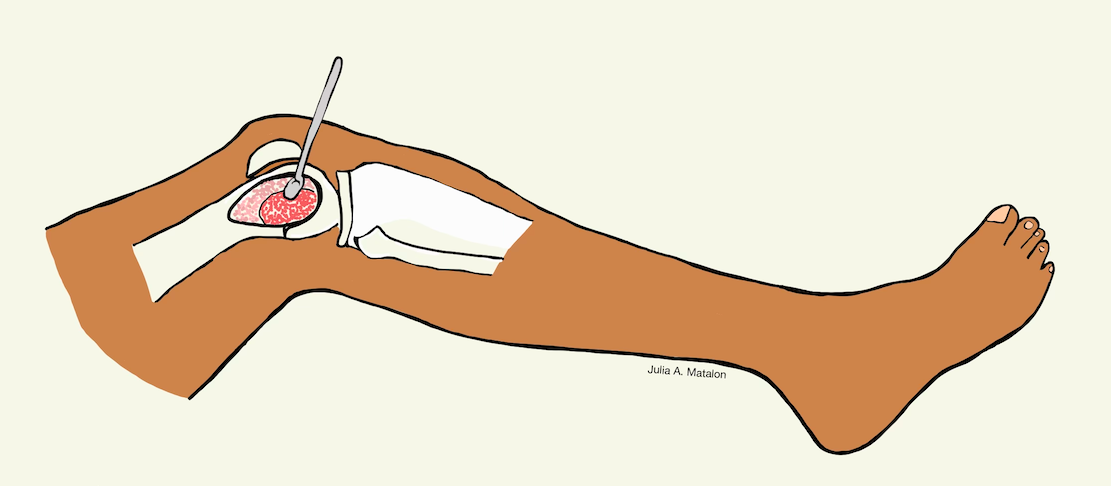
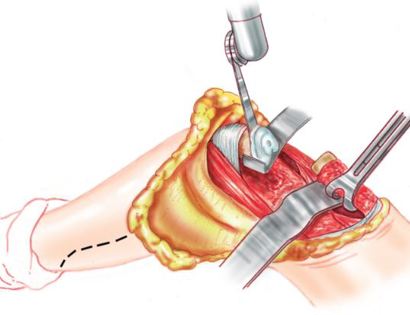
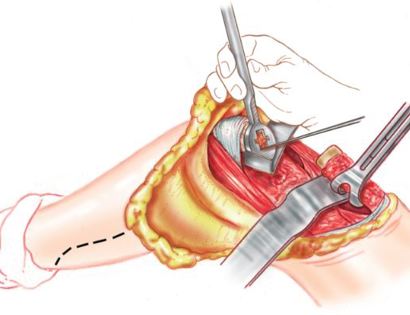
The incision is made, containing the marked biopsy site, along with margins so no tumor remains after it is removed.
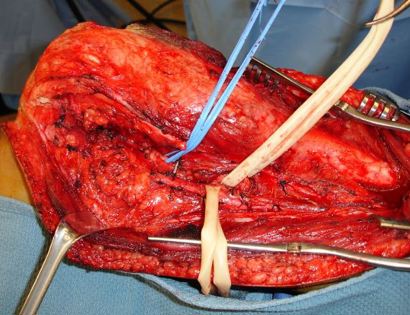
Developing surgical planes (margins that are tumor free) and separating muscles that can be preserved and leaving those in continuity with the tumor that should be removed. This is based on preoperative MRI and intraoperative findings as well as the type of tumor.
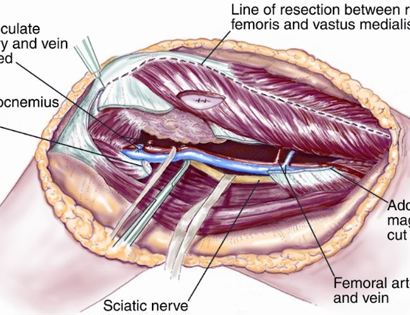
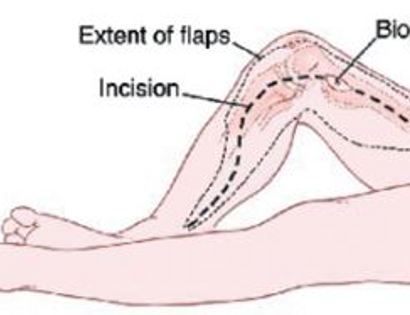
Separating all major arteries, veins, and nerves from the tumor. In rare cases a nerve (s) may need to be removed if it is involved by the bone sarcoma. For this procedure it is vital that the femoral vessels (femur artery and veins), popliteal vessels (arteries and veins around your knee joint), and sciatic nerve are properly identified. Once the blood vessels and nerves are properly identified they can be retracted (moved away) and protected throughout the procedure.
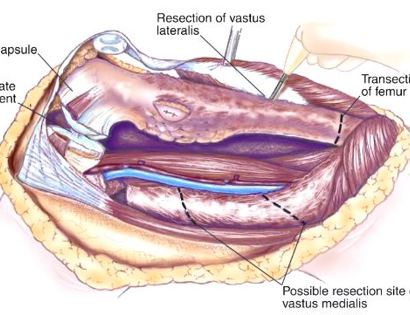
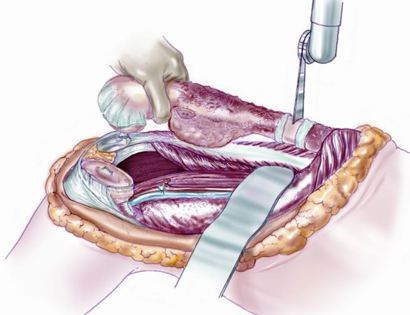
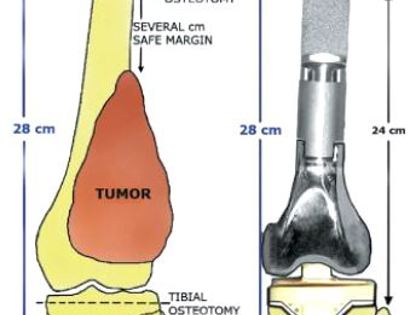
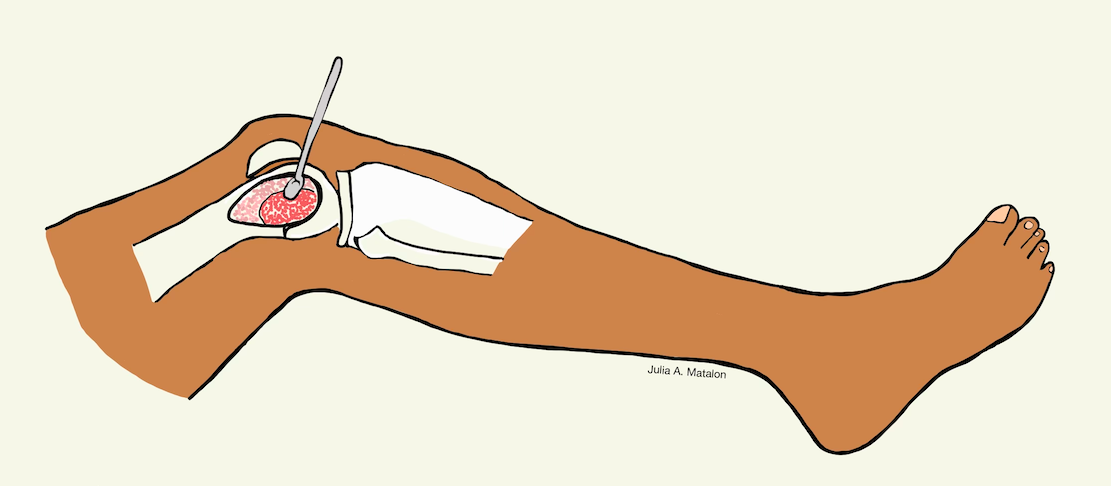
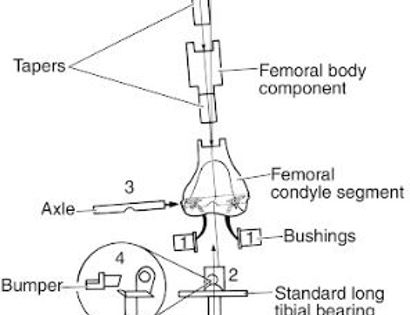
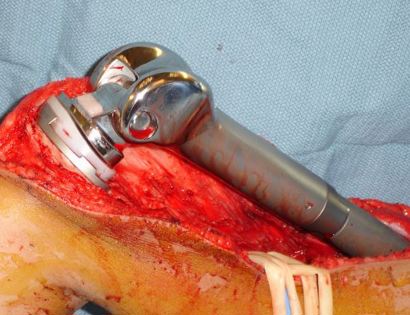
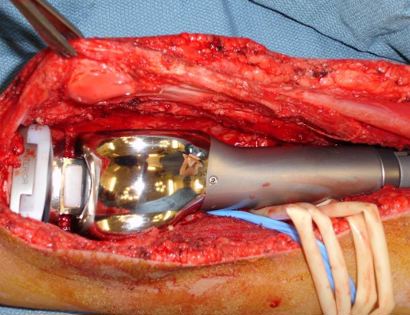
Removal of tumor and reconstruction with a tumor prosthesis. Reconstruction of the lower leg/knee utilizing a specialized tumor prosthesis is the most common limb-sparing technique for bone sarcomas, soft-tissue sarcomas, or large benign aggressive tumors that have destroyed the bone arising in this area. This prosthesis is sized and built during the surgical procedure then implanted and secured in place using cement. The length of bone removed is based on preoperative X-rays and MRI.
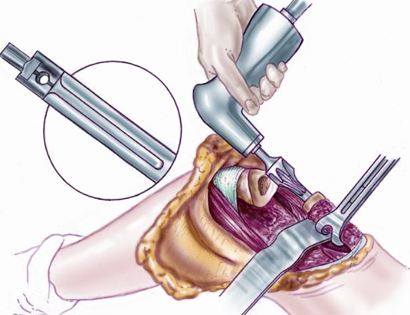

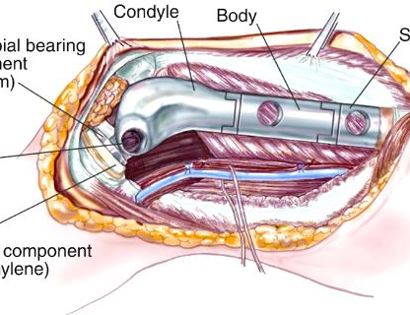
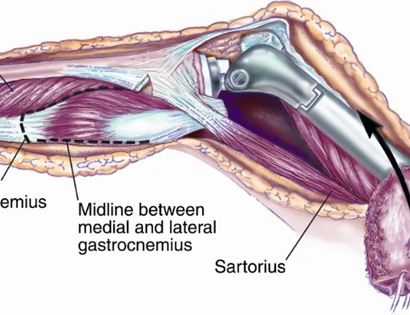
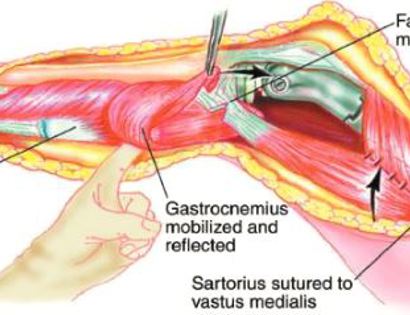
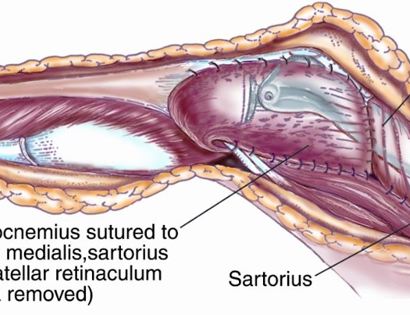
Soft tissue coverage of the prosthesis. Multiple muscle rotation flaps are used to restore function and stability of the knee as best as possible. The goal is to provide a stable knee so the extremity can function well. Soft-tissue reconstruction that involves rotating and reattaching the surrounding muscles, including the gastrocnemius (calf muscle) and vastus medialis (quadriceps muscle). Restoring the function of the surrounding muscles and knee joint is most important for achieving optimal functional outcomes and for protecting the prosthesis from infection.
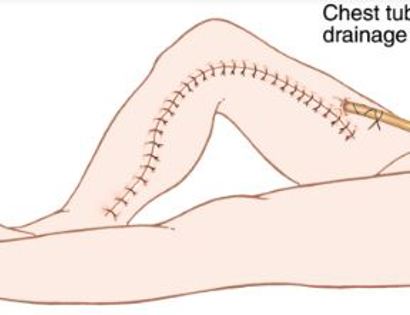
We then close your incision with sutures and cover the surgical site with bandages. Multiple large drains may also be used to drain the surgical site and prevent a seroma (buildup of fluid).







After your surgery you may spend a few nights in the hospital depending on the type of surgery. Once discharged from the hospital, you will be recuperating at home. Various pain protocols and nerve blocks are used to minimize pain. Mostly all patients are very comfortable after the surgery. For the first few days you will ice the area and keep it elevated to reduce swelling. You will return to the office 2 weeks after surgery. Once cleared, you may subsequently start physical therapy depending on the extent of your procedure. We usually prescribe specific physical therapy protocols 3 times a week for 12 weeks after surgery to gradually strengthen muscles. Strengthening with significant resistance after sufficient range of motion is achieved as determined by Dr. Wittig. There may be an ultimate weight limit imposed upon you depending on various factors.
You will be monitored periodically with X-Ray and MRI imaging over the course of 5 years to ensure there are no signs of recurrence. You will have follow up appointments every 4 months for the first 2 years, then every 6 months for the next 2 years, and then once a year. Since the integrity of the limb has been restored to full or almost full, recovery is anticipated provided the patient adheres to strict physical therapy.

Dr. James Wittig narrates a video illustrating the surgical technique for the resection of a bone sarcoma. | WATCH VIDEO